Challenges and advances in anti-rabies vaccine development in sub-saharan Africa
Authors
-
M. C. Owosen
Microbiology Department, Federal University of Lafia, P.M.B. 146, Lafia, Nasarawa State, Nigeria
-
A. W. Jik
Microbiology Department, Federal University of Lafia, P.M.B. 146, Lafia, Nasarawa State, NigeriaNational Veterinary Research Institute, Vom, Nigeria
-
D. D. Odonye
Microbiology Department, Federal University of Lafia, P.M.B. 146, Lafia, Nasarawa State, Nigeria
-
E. B. Ogundeji
National Veterinary Research Institute, Vom, Nigeriahttps://orcid.org/0009-0002-6712-0165
Keywords:
Rabies, Anti-rabies, Vaccine, Sub-saharan AfricaAbstract
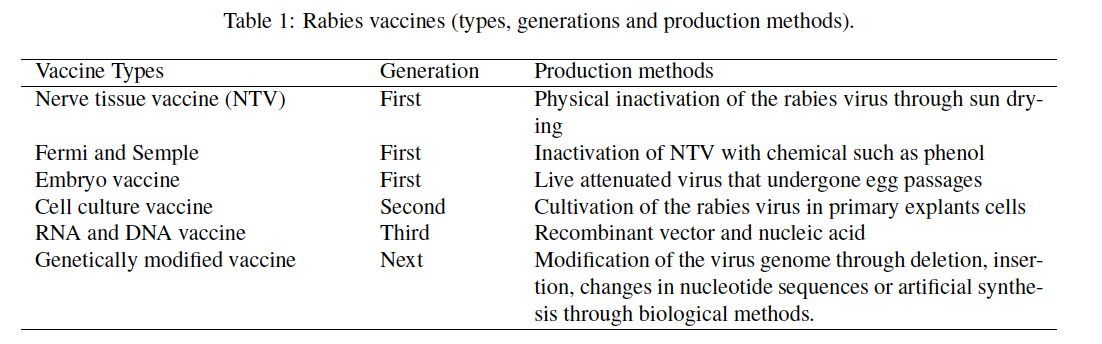
Zoonotic infection, such as rabies disease, causes devastating brain disorders. Rabies causes almost 100 % fatality rate in humans, and it is also 100 % preventable. Thousands of people die from rabies each year, with the majority occurring in Sub-Saharan Africa.The disease is one of the deadliest viral diseases known to humans, which claims about 60,500 human lives annually, mostly in countries with low income. Over 90 % of rabies infections are transmitted via dogs.Rabies vaccines are the major means to prevent and tocontrol rabies.The vaccines can be administered both pre- and post-exposure prophylaxis.The rabies vaccine was first developed witha virus-infected nerve tissue. In its evolutional stages, different types of vaccines have evolved, such as toxoid vaccines, live attenuated vaccines, inactivated vaccines and subunit vaccines. Future trends of novel vaccines development are targeted towards nuclei-based vaccine and therapeutic vaccine for specific diseases. These advances in technology arelimited in Sub-Saharan Africa, owing to lack of infrastructure, high cost low power supply and economic constraint. The vaccine market size is small, and those with the greatest need for vaccine, cannot afford to purchase them at market price.The delivery systems remain another important area of focus, which when addressed will help in effective shipping and access of the product. This review examines the key challenges and recent advances in addressing vaccine development in Sub-Saharan Africa, with the aim of highlighting effective strategies to improve vaccine quality and acceptance coverage.
[1] R. Singh, K. P. Singh, S. Cherian, M. Saminathan, S. Kapoor, S. Manjunatha & G. B. Reddy, “Rabies epidemiology, pathogenesis, public health concerns and advances in diagnosis and control: a comprehensive review”, Vet Q 37 (2017) 212. https://doi.org/10.1080/01652176.2017.1343516.
[2] P. J. Walker, J. Freitas-Astúa, N. Bejerman, K. R. Blasdell, R. Breyta, R. G. Dietzgen, A. R. Fooks, H. Kondo, G. Kurath, I. V. Kuzmin, “ICTV virus taxonomy profile: Rhabdoviridae”, J Gen Virol 103 (2022) 10. http://doi.org/10.1099/jgv.1001689.
[3] A. Bahiru, W. Molla, L. Yizengaw, S. A. Mekonnen, W. T. Jemberu & A. Bahiru, “Knowledge, attitude and practice related to rabies among residents of Amhara region, Ethiopia”, Heliyon 8 (2022) e11366. https://doi.org/10.1016/j.heliyon.2022.e11366.
[4] E. Kenu, V. Ganu, C. L. Noora, R. Adanu & M. Lartey, “Management of dog bites by frontline service providers in primary health-care facilities in the Greater Accra Region of Ghana, 2014–2015”, Infect Dis Poverty 7 (2018) 18. https://link.springer.com/doi/10.1186/s40249-018-0398-3.
[5] World Health Organization, “Rabies”, (2020). https://www.who.int/news-room/fact-sheets/detail/rabies.
[6] World Health Organization, “Rabies, countries or areas at risk”, 2013. Available [Online]. https://www.woah.org/en/home/.
[7] A. C. Jackson, “Human rabies”, Curr Infect Dis Rep 18 (2016) 38. https://doi.org/10.1007/s11908-016-0540-y.
[8] Y. J. Atuman, A. B. Ogunkoya, D. A. Y. Adawa, A. J. Nok & M. B. Biallah, “Dog ecology, dog bites and rabies vaccination rates in Bauchi State, Nigeria”, Int J Vet Sci Med 2 (2014) 41. https://doi.org/10.1016/j.ijvsm.2014.04.001.
[9] M. Kaur, R. Garg, S. Singh & R. Bhatnagar, “Rabies vaccines: where do we stand, where are we heading?”, Expert Rev Vaccines 14 (2015) 369. https://doi.org/10.1586/14760584.2015.973403.
[10] D. K. Yang, H. H. Kim, S. S. Choi, J. T. Kim, W. H. Jeong & J. Y. Song, “Oral immunization of mice with recombinant rabies vaccine strain (ERAG3G) induces complete protection”, Clin Exp Vaccine Res 4 (2015) 107. https://doi.org/10.7774/cevr.2015.4.2.107.
[11] A. R. Fooks, F. Cliquet, S. Finke, C. Freuling, T. Hemachudha, R. S. Mani, T. Müller, S. Nadin-Davis, E. Picard-Meyer & H. Wilde, “Rabies”, Nat Rev Dis Primers 3 (2017) 17091. https://doi.org/10.1038/nrdp.2017.91.
[12] A. Tarantola, M. C. Tejiokem & D. J. Briggs, “Evaluating new rabies post-exposure prophylaxis (PEP) regimens or vaccines”, Vaccine 37 (2019) 88. https://doi.org/10.1016/j.vaccine.2018.10.103.
[13] Global Alliance for Rabies Control, “Working to eliminate human deaths from dog rabies by 2030”, 2017. Available [Online]. https://rabiesalliance.org/country/nigeria.
[14] World Organization for Animal Health, “Global strategic plan to end human deaths from dog-mediated rabies by 2030”, (2018). http://www.who.int/rabies/resources/9789241513838/en.
[15] N. Krithiga, I. Shrikrishna, V. Balamurugan, R. Sharada, D. Rathnamma & R. F. Anthony, “Developments in rabies vaccines: the path traversed from Pasteur to the modern era of immunization”, Vaccines 11 (2023) 756. https://doi.org/10.3390/vaccines11040756.
[16] A. El-Sayed, “Advances in rabies prophylaxis and treatment with emphasis on immunoresponse mechanisms”, Int J Vet Sci Med 6 (2018) 8. https://doi.org/10.1016/j.ijvsm.2018.05.001.
[17] S. Zhu & C. Guo, “Rabies control and treatment: from prophylaxis to strategies with curative potential”, Viruses 8 (2016) 279. https://doi.org/10.3390/v8110279.
[18] R. Cid & J. Bolivar, “Platforms for production of protein-based vaccines: from classical to next-generation strategies”, Biomolecules 11 (2021) 1072. https://doi.org/10.3390/biom11081072.
[19] T. Tantawichien & C. E. Rupprecht, “Modern biologics for rabies prophylaxis and the elimination of human cases mediated by dogs”, Expert Opin Biol Ther 20 (2020) 1347. https://doi.org/10.1080/14712598.2020.1766021.
[20] G. Yale, M. Lopes, S. Isloor, J. R. Head, S. Mazeri, L. Gamble, K. Dukpa, G. Gongal & D. Gibson, “Review of oral rabies vaccination of dogs and its application in India”, Viruses 14 (2022) 155. https://doi.org/10.3390/v14010155.
[21] G. Gongal & G. Sampath, “Introduction of intradermal rabies vaccination—a paradigm shift in improving post-exposure prophylaxis in Asia”, Vaccine 37 (2019) A94. https://doi.org/10.1016/j.vaccine.2018.08.034.
[22] K. Hampson, L. Coudeville, T. Lembo, M. Sambo, A. Kieffer, M. Attlan, J. Barrat, J. D. Blanton, D. J. Briggs & S. Cleaveland, “Estimating the global burden of endemic canine rabies”, PLoS Negl Trop Dis 9 (2015) e0003709. https://doi.org/10.1371/journal.pntd.0003709.
[23] S. Rajendra, P. S. Karam, C. Susan, S. Mani, K. Sanjay, R. Manjunatha & P. Shibani, “Rabies - epidemiology, pathogenesis, public health concerns and advances in diagnosis and control: a comprehensive review”, Vet Q 37 (2017) 212. https://doi.org/10.1080/01652176.2017.1343516.
[24] P. P. Mshelbwala, E. R. Charles, O. O. Modupe, O. N. Emmanuel, G. O. Terese, J. W. Scott & J. C. Nicholas, “Factors influencing canine rabies vaccination among dog-owning households in Nigeria”, One Health 18 (2024) 100751. https://doi.org/10.1016/j.onehlt.2024.100751.
[25] X. Wu, T. G. Smith & C. E. Rupprecht, “From brain passage to cell adaptation: the road of human rabies vaccine development”, Expert Rev Vaccines 10 (2011) 1597. https://doi.org/10.1586/erv.11.140.
[26] S. Rourou, Y. Ben Ayed, K. Trabelsi, S. Majoul & H. Kallel, “An animal component free medium that promotes the growth of various animal cell lines for the production of viral vaccines”, Vaccine 32 (2014) 2767. https://doi.org/10.1016/j.vaccine.2014.02.040.
[27] K. Dhama, S. Chakraborty, M. Y. Mahima, A. K. Verma, R. Deb, R. Tiwari & S. Kapoor, “Novel and emerging therapies safeguarding health of humans and their companion animals: a review”, Pak J Biol Sci 16 (2013) 101. https://doi.org/10.3923/pjbs.2013.101.111.
[28] Tenzin & M. P. Ward, “Review of rabies epidemiology and control in South, South East and East Asia: past, present and prospects for elimination”, Zoonoses Public Health 59 (2012) 451. https://doi.org/10.1111/j.1863-2378.2012.01489.x.
[29] A. Velasco-Villa, L. E. Escobar, A. Sanchez, M. Shi, D. G. Streicker, N. F. Gallardo-Romero, F. Vargas-Pino, V. Gutierrez-Cedillo, I. Damon & G. Emerson, “Successful strategies implemented towards the elimination of canine rabies in the Western Hemisphere”, Antiviral Res 143 (2017) 1. https://doi.org/10.1016/j.antiviral.2017.03.023.
[30] H. Wilde, T. Hemachudha, S. Wacharapluesadee & B. Lumlertdacha, “Rabies in Asia: the classical zoonosis”, in One health: the human-animal-environment interfaces in emerging infectious diseases, Springer, Berlin, Germany, 2013, pp. 185. https://doi.org/10.1007/82 2012228.
[31] D. K. Yang, I. S. Cho & H. H. Kim, “Strategies for controlling dog-mediated human rabies in Asia: using ”One Health” principles to assess control programmes for rabies”, Rev Sci Tech 37 (2018) 473. https://doi.org/10.20506/rst.37.2.2816.
[32] C. Mbilo, J. B. Kabongo, P. P. Pyana, L. Nlonda, R. W. Nzita & B. Luntadila, “Do ecology, bite incidence, and disease awareness: a cross-sectional survey among a rabies-affected community in the Democratic Republic of the Congo”, Vaccines (Basel) 7 (2019) 98. https://doi.org/10.3390/vaccines7030098.
[33] L. Konzing, J. Kwaga, G. Kia & H. A. Kazeem, “A retrospective study of dog bite cases reported to some hospitals in Plateau State, Nigeria”, Sokoto J Vet Sci 17 (2019) 56. https://doi.org/10.4314/sokjvs.v17i1.7.
[34] N. Caffrey, M. Rock, O. Schmidt, D. Anderson, M. Parkinson & S. L. Checkley, “Insights about the epidemiology of dog bites in a Canadian city using a dog aggression scale and administrative data”, Animals (Basel) 9 (2019) 324. https://doi.org/10.3390/ani9060324.
[35] I. Tekki, C. Meseko, S. Omotainse, Y. Atuman, S. Olaleye & P. Okewole, “Incidences of rabies in domestic animals and consequent risk factors in humans”, J Med Microbiol Diagn 3 (2014) 1. https://doi.org/10.4172/2161-0703.1000143.
[36] P. P. Mshelbwala, J. S. Weese, O. A. Sanni-Adeniyi, S. Chakma, S. S. Okeme, A. A. Mamun, C. E. Rupprecht & R. J. S. Magalhaes, “Rabies epidemiology, prevention and control in Nigeria: scoping progress towards elimination”, PLoS Negl Trop Dis 15 (2021) e0009617. https://doi.org/10.1371/journal.pntd.0009617.
[37] M. Kaur, R. Garg, S. Singh & R. Bhatnagar, “Rabies vaccines: where do we stand, where are we heading?”, Expert Rev Vaccines 14 (2015) 369. https://doi.org/10.1586/14760584.2015.973403.
[38] J. E. Norton, A. G. Lytle, S. Shen, E. P. Tzvetkov, C. L. Dorfmeier & J. P. McGettigan, “ICAM1-based rabies virus vaccine shows increased infection and activation of primary murine B cells in vitro and enhanced antibody titers in vivo”, PLoS One 9 (2014) e87098. https://doi.org/10.1371/journal.pone.0087098.
[39] P. Vescovo, N. Rettby, N. Ramaniraka, J. Liberman, K. Hart, A. Cachemaille, L. D. Piveteau, R. Zanoni, P. A. Bart & G. Pantaleo, “Safety, tolerability and efficacy of intradermal rabies immunization with DebioJect™”, Vaccine 35 (2017) 1782. https://doi.org/10.1016/j.vaccine.2016.09.069.
[40] F. Qin, F. Xia, H. Chen, B. Cui, Y. Feng, P. Zhang, J. Chen & M. A. Luo, “Guide to nucleic acid vaccines in the prevention and treatment of infectious diseases and cancers: from basic principles to current applications”, Front Cell Dev Biol 9 (2021) 633776. https://doi.org/10.3389/fcell.2021.633776.
[41] N. Ito, T. Okamoto, M. Sasaki, S. Miyamoto, T. Takahashi, F. Izumi, M. Inukai, S. Jarusombuti, K. Okada & K. Nakagawa, “Safety enhancement of a genetically modified live rabies vaccine strain by introducing an attenuating Leu residue at position 333 in the glycoprotein”, Vaccine 39 (2021) 3777. https://doi.org/10.1016/j.vaccine.2021.05.002.
[42] U. Molini, R. Hassel, S. Ortmann, A. Vos, M. Loschke, A. Shilongo & C. M. Freuling, T. Müller, “Immunogenicity of the oral rabies vaccine strain SPBN GASGAS in dogs under field settings in Namibia”, Front. Veterinary Science 8 (2021) 1224. https://doi.org/10.3389/fvets.2021.737250.
[43] R. Li, L. Huang, J. Li, Z. Mo, B. He, Y. Wang, X. Wu, M. Minutello, F. Guinet-Morlot & S. Pichon, “A next-generation, serum-free, highly purified vero cell rabies vaccine is safe and as immunogenic as the reference vaccine verorab when administered according to a post-exposure regimen in healthy children and adults in China”, Vaccine 31 (2013) 5940. https://doi.org/10.1016/j.vaccine.2013.10.043.
[44] D. K. Yang, H. H. Kim, K. W. Lee & J. Y. Song, “The present and future of rabies vaccine in animals”, Clinical Exp. Vaccine Research 2 (2013) 19. https://doi.org/10.7774/cevr.2013.2.1.19.
[45] A. Regalado, “The U.S. government has begun testing its first zika vaccine in human”, (2016). https://www.cphi-online.com/news/research-and-development.html.
[46] Y. Chen & S. Wang, S. Lu, “DNA immunization for HIV vaccine development”, Vaccines 2 (2024) 138. https://doi.org/10.3390/vaccines2010138.
[47] K. Katalin & W. Drew, “Awarded horwitz prize for pioneering research on convid-19 vaccines”, Columbia University Irving Medical Center (2021). https://www.cuimc.columbia.edu/news/horwitz-prize-2021.
[48] E. S. Starodubova, O. V. Preobrazhenskaia, Y. V. Kuzmenko, A. A. Latanova, E. I. Yarygina & V. L. Karpov, “Rabies vaccines: Current status and prospects for development”, Molecular Biology 49 (2015) 577. https://doi.org/10.7868/S0026898415040175.
[49] C. E. Rupprecht, C. A. Hanlon & T. Hemachudha, “Rabies reexamined”, Lancet Infectious Disease 2 (2002) 327. https://doi.org/10.1016/S1473-3099(02)00287-6.
[50] A. Giesen, D. Gniel & C. Malerczyk, “30 years of rabies vaccination with rabipur: A summary of clinical data and global experience”, Expert Rev Vaccines 14 (2015) 351. https://doi.org/10.1586/14760584.2015.1011134.
[51] P. Admasu & Y. Mekonnen, “Rabies and its folk drugs remedies in Ethiopia: A review”, International Journal of Basic and Applied Virology 3 (2014) 22. https://doi.org/10.5829/idosi.ijbav.2014.3.2.8332.
[52] A. Mesfin, T. Wogayehu, A. Amelework, A. Sintayehu, G. Garuma, H. Alemnesh, T. Yirgalem, K. Gutu, B. Endalkachew, F. Ibsa, G. Abebe & M. Yimer, “Situation of rabies in Ethiopia: A five-year retrospective study of human rabies in addis ababa and the surrounding regions”, Journal of Tropical Medicine 2021 (2021) 6662073. https://doi.org/10.1155/2021/6662073.
[53] K. L. O’Brien & T. Nolan, “WHO position on rabies immunization - 2018 updates”, Vaccine 37 (2019) A85. https://doi.org/10.1016/j.vaccine.2018.10.014.
[54] L. Shuai, N. Feng, X. Wang, J. Ge, Z. Wen, W. Chen, L. Qin, X. Xia & Z. Bu, “Genetically modified rabies virus ERA strain is safe and induces long-lasting protective immune response in dogs after oral vaccination”, Antiviral Res 121 (2015) 9. https://doi.org/10.1016/j.antiviral.2015.06.011.
[55] G. Galvez-Romero, M. Salas-Rojas, E. N. Pompa-Mera, K. Chávez-Rueda & A. Aguilar-Setién, “Addition of C3d-P28 adjuvant to a rabies DNA vaccine encoding the G5 linear epitope enhances the humoral immune response and confers protection”, Vaccine 36 (2018) 292. https://doi.org/10.1016/j.vaccine.2017.11.047.
[56] D. K. Yang, H. H. Kim, K. W. Lee & J. P. Song, “The present and future of rabies vaccine in animals”, Clinical and Experimental Vaccine Research 2 (2013) 19. https://doi.org/10.7774/cevr.2013.2.1.19.
[57] X. Wu, T. G. Smith & C. E. Rupprecht, “From brain passage to cell adaptation: The road of human rabies vaccine development”, Expert Review of Vaccines 10 (2011) 1597. https://doi.org/10.1586/erv.11.140.
[58] A. Saleh, S. Qamar, A. Tekin, R. Singh & R. Kashyap, “Vaccine development throughout history”, Cureus 13 (2021) e16635. https://doi.org/10.7759/cureus.16635.
[59] S. Rourou, Y. Ben Ayed, K. Trabelsi, S. Majoul & H. Kallel, “An animal component free medium that promotes the growth of various animal cell lines for the production of viral vaccines”, Vaccine 32 (2014) 2767. https://doi.org/10.1016/j.vaccine.2014.02.040.
[60] H. Birhanu, T. Belete, N. Dagmar, M. Abebe & K. Gezahegn, “Safety and immunogenicity of ethiorab rabies vaccine”, Journal of Vaccines & Vaccination 4 (2013) e117. https://doi.org/10.4172/2157-7560.1000e117.
[61] G. Tefera, E. Yimer & A. Geyid, “Endemic existence of rabies in Ethiopia”, Ethiopian Medical Journal 40 (2002) 163. https://eurekamag.com/research/003/750/003750147.php.
[62] E. Olayan, M. El-Khadragy, A. F. Mohamed, A. K. Mohamed, R. I. Shebl & H. M. Yehia, “Evaluation of different stabilizers and inactivating compounds for the enhancement of vero cell rabies vaccine stability and immunogenicity: In vitro study”, BioMed Research International 2019 (2019) 4518163. https://doi.org/10.1155/2019/4518163.
[63] G. Gongal & G. Sampath, “Introduction of intradermal rabies vaccination - A paradigm shift in improving post-exposure prophylaxis in Asia”, Vaccine 37 (2019) A94. https://doi.org/10.1016/j.vaccine.2018.08.034.
[64] R. E. Kissling & D. R. Reese, “Anti-rabies vaccine of tissue culture origin”, Journal of Immunology 91 (1963) 362. https://doi.org/10.4049/jimmunol.91.3.362.
[65] R. Shipley, E. Wright, F. Z. X. Lean, D. Selden, D. L. Horton, A. R. Fooks & A. C. Banyard, “Assessing rabies vaccine protection against a novel lyssavirus, kotalahti bat lyssavirus”, Viruses 13 (2021) 947. https://doi.org/10.3390/v13050947.
[66] J. Maki, A. L. Guiot, M. Aubert, B. Brochier, F. Cliquet, C. A. Hanlon, R. King, E. H. Oertli, C. E. Rupprecht & C. Schumacher, “Oral vaccination of wildlife using a vaccinia-rabies-glycoprotein recombinant virus vaccine (Raboral V-RG): A global review”, Veterinary Research 48 (2017) 57. https://doi.org/10.1186/s13567-017-0459-9.
[67] J. Guo, M. Mondal & D. Zhou, “Development of novel vaccine vectors: Chimpanzee adenoviral vectors”, Human Vaccines & Immunotherapeutics 14 (2018) 1679. https://doi.org/10.1080/21645515.2017.1419108.
[68] F. Napolitano, R. Merone, A. Abbate, V. Ammendola, E. Horncastle, F. Lanzaro, A. Esposito, E. I. Latanova, V. L. Yarygina, M. Karpov, A. M. Contino, R. Sbrocchi & A. Sommella, “Correction: A next generation vaccine against human rabies based on a single dose of a chimpanzee adenovirus vector serotype C”, PLoS Neglected Tropical Disease 15 (2021) e0009348. https://doi.org/10.1371/journal.pntd.0009348.
[69] C. Li, Y. Wang, H. Liu, X. Zhang, D. Baolige, S. Zhao, W. Hu & Y. Yang, “Change in the single amino acid site 83 in rabies virus glycoprotein enhances the BBB permeability and reduces viral pathogenicity”, Frontiers in Cell and Developmental Biology 8 (2021) 632957. https://doi.org/10.3389/fcell.2020.632957.
[70] M. Sambo, S. Cleaveland & H. Ferguson, “The burden of rabies in Tanzania and its impact on local communities”, PLoS Neglected Tropical Diseases 7 (2013) e2510. https://doi.org/10.1371/journal.pntd.0002510.
[71] D. O. Osaghae, “Animal and human bites in children”, West African Journal of Medicine 30 (2011) 421. https://www.ajol.info/index.php/wajm/issue/view/10724.
[72] T. I. Isek, J. Umoh & A. A. Dzikwi, “A retrospective study of dog bite occurrence and anti-rabies vaccination of dogs in a state veterinary hospital in Ogoja, Cross River State, Nigeria”, Veterinaria Italiana 55 (2019) 163. https://doi.org/10.12834/VetIt.150.431.5.
[73] A. Stokes, J. Pion, O. Binazon, B. Laffont, M. Bigras, G. Dubois, K. Blouin, J. K. Young, M. A. Ringenberg & N. Ben Abdeljelil, “Nonclinical safety assessment of repeated administration and biodistribution of a novel rabies self-amplifying mRNA vaccine in rats”, Regulatory Toxicology and Pharmacology 113 (2020) 104648. https://doi.org/10.1016/j.yrtph.2020.104648.
[74] W. Zhang, N. Cheng, Y. Wang, X. Zheng, Y. Zhao, H. Wang, C. Wang, Q. Han, Y. Gao & J. Shan, “Adjuvant activity of PCP-II, a polysaccharide from poria cocos, on a whole killed rabies vaccine”, Virus Research 270 (2019) 197638. https://doi.org/10.1016/j.virusres.2019.06.001.
[75] T. Jibat, H. Hogeveen & M. C. Mourits, “Review on dog rabies vaccination coverage in Africa: A question of dog accessibility or cost recovery?”, PLoS Negl Trop Dis 9 (2015) e0003447. https://doi.org/10.1371/journal.pntd.0003447.
[76] S. S. Elizaveta, O. V. Preobrazhenskaia & Y. V. Kuzmeko, “Rabies vaccines: Current status and prospects for development”, Molecular Biology 49 (2015) 577. https://doi.org/10.7868/S0026898415040175.
[77] H. I. Koprowski, J. A. Black & D. J. Nelsen, “Studies on chick-embryo-adapted rabies virus”, Journal of Immunology 72 (1954) 79. https://doi.org/10.4049/jimmunol.72.1.79.
[78] H. C. J. Ertl, “New rabies vaccines for use in humans”, Vaccines 7 (2019) 54. https://doi.org/10.3390/vaccines7020054.
[79] T. P. Scott & L. H. Nel, “Rabies prophylactic and treatment options: An in vitro study of siRNA- and aptamer-based therapeutics”, Antiviral Research 123 (2015) 881. https://doi.org/10.1016/j.antiviral.2015.10.002.
[80] S. Prakash, “Development of covid 19 vaccine: A summarized review on global trials, efficacy, and effectiveness on variants”, Diabetes & Metabolic Syndrome: Clinical Research & Reviews 16 (2022) 102482. https://doi.org/10.1016/j.dsx.2022.102482.
[81] Z. Fang, J. Lyu, J. Li, C. Li, Y. Zhang, Y. Guo, Y. Wang, Y. Zhang & K. Chen, “Application of bioreactor technology for cell culture-based viral vaccine production: Present status and future prospects”, Frontiers in Bioengineering and Biotechnology 10 (2022) 921755. https://doi.org/10.3389/fbioe.2022.921755.
[82] Global Alliance for Rabies Control, “Recent research”, 2017. Available [Online]. https://rabiesalliance.org/resource/recent-research-november-2017.
Published
How to Cite
Issue
Section
Copyright (c) 2025 M. C. Owosen, A. W. Jik, D. D. Odonye, E. B. Ogundeji

This work is licensed under a Creative Commons Attribution 4.0 International License.